HealthManagement, Volume 16 - Issue 1, 2016
In any MRI unit, service quality as experienced by patients depends on the design of the care pathway through which the MRI service is delivered (Johnston and Clark 2005; Yazdanparast et al. 2010). Healthcare organisations can create value in terms of improved service quality by developing expertise, reducing errors, increasing efficiency and improving outcomes (Porter and Teisberg 2004). With an ageing population and rising costs, healthcare organisations have adopted quality management systems (QMS) to improve the effectiveness of treatments and increase patient satisfaction with the service. A QMS is a formal process used to review operations, products and services to identify areas of potential quality improvement. It involves a rigorous, iterative process to continually increase the quality and economic value of services. Creating a quality management system requires a strategic decision, input from employees at all levels of an organisation, and is influenced by varying needs, objectives, the products/services provided, the processes employed and the size and structure of the organisation. The successful implementation of QMs could therefore be hindered through lack of coordination between departments, lack of continuous improvement culture and employees' resistance to change.
A question commonly tackled by radiography managers is: how can a service be managed, controlled, measured, reviewed and improved through the collaboration of all stakeholders (including patients)? One way of contributing to this is through an optimised care pathway design, as the latter is crucial for the attainment of an effective, safe and efficient service (Cheah 2000).
The European Pathway Association (e-p-a.org) defines a care pathway as:
A complex intervention for the mutual decision-making and organisation of predictable care for a well-defined group of patients during a well-defined period.
The key characteristics of pathways include:
- An explicit statement of the goals and key elements of
care based on evidence, best practice and patient expectations;
- Facilitation of the communication and coordination of
roles, and sequencing the activities of the multidisciplinary care team,
patients and their relatives;
- Documentation, monitoring and evaluation of variances and
outcomes; and
- Identification of relevant resources.
This project mainly focused on the “facilitation of the communication and coordination of roles, and sequencing the activities of the multidisciplinary care team”. Vanhaecht et al. (2010) describe three different coordination models:
- Chain models: used for relatively highly predictable care processes with a high level of agreement between the team members;
- Hub models: used for less predictable processes with key persons who lead the delivery of the care process;
- Web models: used for highly unpredictable, complex processes.
MRI practice involves a mix of routine and non-routine tasks, where employees need to be able to take initiatives in response to incidental findings, or to optimise processes beyond the confines of standard operating procedures (Ponsignon et al. 2011). The MRI care pathway can be considered as a sub-process that fits a chain model, which permits elements of flexibility.
Within this context if care pathways can be optimised to deliver an effective local service they can also be used to support a quality management system.
A literature search did not locate any studies on the
optimisation of MRI care pathways to support a QMs. discussions with
international MR radiographers indicated that such development is often carried
out using informal methods, which are highly dependent on what is happening
elsewhere are rarely reported in the public domain and the validities of which
are therefore rarely open to scrutiny; in addition, care pathways need to be
specific to local healthcare needs and culture.
The purpose of this project was to bring together a multistakeholder, interprofessional expert group to develop further and optimise an MRI care pathway model to support an MRI regional quality management system.
Method
Various techniques were considered for the participation of the multi-stakeholder expert group. A literature survey revealed that multi-stakeholder processes that require consensus techniques include the Delphi, nominal group or focus group techniques (Jones and Hunter 1995; Hutchings et al. 2006; Kitzinger 1995). For this study the researchers opted for the nominal group technique (NGT), because the approach allows an adequate number of MRI stakeholders, who could meet in one sitting and voice their opinions freely. To kick-start the process an initial model of the MR care pathway for adults was developed by a small multidisciplinary group comprising an MRI radiographer, radiologist and medical physicist and forwarded to the participants. This ensured that the participants focused on the actual pathway during the NGT process proper. The NGT method used in this study is published elsewhere (Castillo et al. 2015).
Seventeen participants, representing radiologists, radiographers, management, medical physicists, policymakers, physiotherapists and nurses working in orthopaedics, neurosurgery and neurology were invited to create a balanced representation of expertise. Ideally the group of participants should also have included patient representatives, but since these are still very much in their infancy in Malta, nurses working in neurology and orthopaedic wards were invited to participate as patient advocates. This had the added advantage that bias resulting from power inequalities between patients and healthcare professionals was avoided (Vaartio-Rajalin and Leino-Kilpi 2011). Ethical approval was received from the ethics committee of the University of Malta. All participants were provided with information regarding the study, and consent was obtained before the start of the NGT.
Results
Fourteen participants accepted the invitation to participate: an executive from the principal public general hospital, a manager from the national Ministry for health, a service development manager from the allied healthcare professional sector, 2 senior physiotherapists, 3 nursing officers, 3 MRI radiographers, 2 medical physicists and 1 radiologist. The NGT process resulted in ten issues, which were determined by ranking scores assigned by the participants. These are shown in Table 1 in decreasing order of importance (the latter quantified using a ranking score).
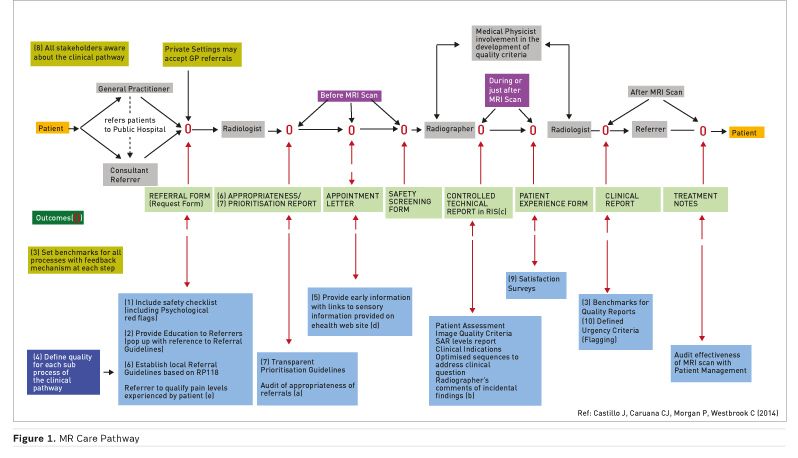
The group gave a strong affirmative answer when asked if the model as presented by the researchers with the additional 10 issues identified through the NGT was sufficient to form the basis of the desired future MR care pathway. The resulting MR care pathway is shown in Figure 1. The pathway shows the patient’s journey from when he/she is referred for an MRI scan up to the follow-up visit to the referrer. The numbers in brackets (1- 10) in the diagram refer to the NGT-identified issues from table 1 relevant to that particular section of the pathway. The pathway is divided into various sub-processes at which defined quality outcomes (indicated with an ‘O’ in the diagram) and associated criteria would need to be inserted.
the following additional suggestions gleaned from the verbatim transcript of the session, which add further support for the main issues of Table 1 were also incorporated into the care pathway (indicated as (a) – (e) in the diagram):
a. Need for a mechanism to audit the appropriateness of referrals. “We need to answer the question: has the investigation had an effect on patient management? We are all aware of the high percentage of patients being referred simply because the referrer has no other option - patients insist on an MRI even on occasions when the referrer thinks it is inappropriate.”
b. Need to educate radiographers on procedures to follow for incidental findings: “Although there is an electronic feedback mechanism linking radiographers and radiologists this is not always being utilised owing to the large throughput.”
c. Importance of the introduction of a radiographers’ technical report: “Radiographers should issue a written technical report in which they confirm that the quality of the images was sufficient for diagnosis, and that safety criteriahave been met and to record any variance from the original care plan. This technical report would form the basis for audits….”
d. The use of social electronic media: “We should use social electronic media for providing early explanation to patients on what to expect during an MRI scan.”
e. The importance that the referrer qualifies pain
levels of patients: “The referrer should
qualify the region and level of pain that the patient may be experiencing. This
information would be useful for radiographers to plan the procedure so that the
most important sequences are acquired first in relation to the clinical
question.”
Table 1. Final ranking of the ten most important care pathway optimisation related issues as determined by the participants
| Rank | Items | Remarks | Ranking Score |
| 1 | Safety check at referral stage | This will ensure that any contraindications related to metallic implants are resolved at an early stage, hence eliminating delays on the day of the exam proper (Ferris et al. 2007). Psychological issues that may affect the procedure are brought to the attention of the MRI radiography team in advance (Törnqvist et al. 2006; Grey et al. 2000). This will permit specific anxiety reduction protocols to be employed. | 80 |
| 2 | Education of referrers | MRI education for referring clinicians is necessary to avoid inappropriate requests and better use of MR facilities (Blachar et al. 2006; Lehnert and Bree 2010). | 78 |
| 3 | Establish pre-determined objective quality criteria for evaluation and monitoring at critical stages of the care pathway | Clinical criteria are a standard process adopted by all healthcare organisations that espouse the principles of continuous quality improvement (Busch 2010; Barnes et al. 1994; European Society of Radiology 2002). | 77 |
| 4 | Define in terms of effectiveness, safety and efficiency the meaning of ‘quality’ for each sub-process of the care pathway. | This would ensure that patients receive effective care, in good time and at fair cost (Campbell et al. 2000). | 76 |
| 5 | Early explanation of the procedure to the patient before coming to MRI | An early explanation of the procedure to alleviate anxiety, and identify in advance those patients with claustrophobia is very important (Bolejko et al. 2008; MacKenzie et al. 1995). Early explanation also improves compliance. | 69 |
| 6 | Establish local referral guidelines (appropriateness criteria) | Referral guidelines to assist the referring clinician in choosing the best imaging modality. This issue is a precursor to issue 2 (Lehnert and Bree 2010; Blackmore et al. 2011; Rosenthal et al. 2006). | 66 |
| 7 | Transparent prioritisation guidelines | Transparent prioritisation guidelines to ensure urgent cases are scheduled earlier and non-urgent cases are prioritised fairly and in a transparent manner. System must be transparent so that clinicians will not hinder its implementation and so that patients feel that they have been respected (Emery et al. 2009). | 65 |
| 8 | Knowledge of the care pathway by all stakeholders | This would ensure that the care pathway is accepted by all stakeholders and that any subsequent modifications are well understood and accepted by the various stakeholders (Evans-Lacko et al. 2010). | 55 |
| 9 | Patient satisfaction surveys | Patient satisfaction surveys are today considered as an indispensable tool to provide client feedback for further improvement of service quality (Nelson and Niederberger 1989; Ware 2003). | 50 |
| 10 | Urgency criteria for diagnostic results following the scan (flagging) | In particular critical incidental findings need to be brought to attention of referring clinicians immediately (Singh et al. 2007; Ferris et al. 2009). | 37 |
Discussion
The MR care pathway describes the tasks performed by the various members of the healthcare team as they interact with each other and the patient. The aim is to achieve the desired defined quality outcomes at various stages of the pathway and carry out regular audit to ensure consistent good quality service. The 10 issues and associated quality criteria should be developed into standard operating procedures and included in the QMS. The “remarks” column in Table 1 provides further explanation and discussion relative to the literature, which would also be included in the standard operating procedures.
It is welcome to note the importance given by the participants to patient safety, education of referrers and the communication of urgent and unexpected findings back to referrer (European Society of Radiology 2012). The group has also identified the importance of involving the referrers at an early stage, insisting that the latter should be knowledgeable about the MRI care pathway, and that they should have access to transparent prioritisation guidelines. This would reduce individual barriers to the implementation of the pathway and the quality management system (Evans-Lacko et al. 2010).
Two other important issues are the importance of referral and quality criteria. The Institute of Medicine Committee on Quality of health Care in America referred to underuse, overuse and misuse of care as safety threats to patients at both the individual and collective level (Institute of Medicine 2001). only when compilation, disclosure and evaluation of safety and quality indicators with respect to previously established quality criteria occurs, will the quality of clinical practices be improved (Corrigan 2005). In addition, evaluation should focus not only on end clinical outcomes but also on intermediate sub-processes (Curtis et al. 2006; Von Korff and Goldberg 2001), as proposed in this study. Audit tools in the form of checklists will be developed and used to evaluate key intermediate sub-process outcomes (marked with an ‘O’ in the diagram) that have major impact on end patient outcomes (Vanhaecht et al. 2006).
The group also raised novel issues. Most importantly for the radiography profession, the group suggested the introduction of a technical report by radiographers that together with the radiologist diagnostic report would provide more complete documentation to the referrer and to management. If integrated within the radiology information system this would certainly facilitate the successful implementation of the pathway (Evans-Lacko et al. 2008; Greenhalgh et al. 2004).
Another novel theme raised by the patient advocates was the importance of referrers indicating the level of pain experienced by patients at the time of the MRI scan request. This would permit radiographers to plan a safer and more comfortable imaging strategy for patients. This important suggestion highlights the capacity of healthcare professionals to act on behalf of patients, and the strength of the NGT method in bringing forth previously unknown issues.
Prior information on the MRI procedure for patients should make better use of interactive information technology.
Information about what patients should expect during an MRI procedure would be an effective way of improving the workflow and quality of the service. Although such information is not as widely available as it is desirable, social media are already being used by patients to liaise with medical practitioners and acquire timely information (Hawn 2009).In addition, web-based clinical decision support systems could assist referring clinicians with respect to referral criteria (Kaushal et al. 2003; Rosenthal et al. 2006).
The production of a prioritised list of issues may be seen as a limitation given that the method involved focusing only on the top 10 issues and setting aside those of lower priority. However, this limitation was addressed by asking all participants to silently generate their own list of issues and thus ensure that all issues have an equal probability of being placed on the discussion agenda. This procedure avoided significant risk of loss of important data when more assertive members of the group dominate, effectively excluding the views of others. One can expect a high level of confidence that the group listed the most important items that should be integrated in the pathway. In addition, the process of selection and prioritisation ensured that the issues that were most important to the participants received the highest level of attention. Without this mechanism, there would have been the risk that the discussion be dominated by one or two contentious issues.
Conclusion
This study started from a model of the MR pathway as perceived by a small multidisciplinary group consisting of an MRI radiographer, radiologist and medical physicist, which was in turn subjected to an optimisation process using a nominal group technique. Care pathways are widely believed to be an important tool for ensuring the delivery of high quality, evidence-based care. This paper has presented one example where stakeholders with an interest in MRI and service development came together to contribute to a quality management system. The findings indicate that participants attached the highest importance (rank score >70) to safety, referrer education and defining quality criteria. The NGT method also brought forward novel themes, in particular the need for a radiographer’s technical report and the need for referrers to indicate pain levels of patients. The care pathway would provide the necessary data to monitor the service quality. The pathway is considered as a living document and would require periodic ongoing re-evaluation in an iterative process.
Note
The complete study has been published elsewhere (Castillo et al. 2015) dx.doi.org/10.1016/j.radi.2014.09.002
Conflict of interest: None
Key Points
- Optimisation of an MRI
care pathway by a multi-stakeholder expert group.
- Introduction of a
radiographer’s technical report as an assessment of image quality.
- Establish quality criteria at each step of the pathway for audit purposes.
See Also: New Ways of Optimising Imaging Services
References:
Barnes R, Lawton L, Briggs D (1994) Clinical benchmarking improves clinical paths: experience with coronary artery bypass grafting. Jt Comm J Qual Improv, 20(5): 267-76.
Blachar A, Tal S, Mandel A et al. (2006) Preauthorization of CT and MRI examinations: assessment of a managed care preauthorization program based on the ACR appropriateness criteria and the Royal College of Radiology guidelines. J Am Coll Radiol, 3(11): 851-9.
Blackmore CC, Mecklenburg RS, Kaplan GS (2011) Effectiveness of clinical decision support in controlling inappropriate imaging. J Am Coll Radiol, 8(1): 19-25.
Bolejko A, Sarvik C, Hagell P et al. (2008) Meeting patient information needs before magnetic resonance imaging: development and evaluation of an information booklet. Journal of Radiology Nursing, 27(3): 96-102.
Busch HP (2010) [Benchmarking of radiological departments--starting point for successful process optimization] RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin, 182(3): 221-8.
Campbell SM, Roland MO, Buetow SA (2000) Defining quality of care. Soc Sci Med, 51(11): 1611-25.
Castillo J, Caruana CJ, Morgan PS et al. (2015) Optimizing a magnetic resonance care pathway: a strategy for radiography managers. Radiography, 21(1): e29-e33.
Cheah J (2000) Development and implementation of a clinical pathway programme in an acute care general hospital in Singapore. Int J Qual Health Care,12(5): 403-12.
Corrigan JM (2005) Crossing the quality chasm. In: Reid PP, Compton WD, Grossman JH, et al, eds. Building a better delivery system: a new engineering/ health care partnership. Washington, DC: National Academies Press.
Curtis JR, Cook DJ, Wall RJ et al. (2006) Intensive care unit quality improvement: a" how-to" guide for the interdisciplinary team. Crit Care Med, 34(1): 211-8.
Emery DJ, Forster AJ, Shojania KG et al. (2009) Management of MRI wait lists in Canada. Healthc Policy, 4(3): 76-86.
European Society of Radiology (ESR) (2012) ESR guidelines for the communication of urgent and unexpected findings. Insights Imaging, 3(1): 1-3.
European Society of Radiology (ESR) (2002) Benchmarking radiological services in Europe. [Accessed: 3 February 2016] Available from myesr.org/html/img/pool/Benchmarking_radiological_services_in_Europe.pdf
Evans-Lacko SE, Jarrett M, McCrone P et al. (2008) Clinical pathways in psychiatry. Br J Psychiatry, 193: 4-5.
Evans-Lacko S, Jarrett M, McCrone P et al. (2010) Facilitators and barriers to implementing clinical care pathways. BMC Health Serv Res, 10: 182.
Ferris NJ, Kavnoudias H, Thiel C et al. (2007) The 2005 Australian MRI safety survey. AJR Am J of Roentgenol, 188(5): 1388-94.
Ferris TG, Johnson SA, Backus M et al. (2009) Electronic results management in pediatric ambulatory care: qualitative assessment. Pediatrics, 123 Suppl 2: S85-91.
Greenhalgh T, Robert G, Bate P et al. (2004) How to spread good ideas. A systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation. Report for the National Co-ordinating centre for NHS Service Delivery and Organisation R & D (NCCSDO), 1-426.
Grey SJ, Price G, Mathews A (2000) Reduction of anxiety during MR imaging: a controlled trial. Mag Reson Imaging, 18(3): 351-5.
Hawn C (2009) Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood),28(2): 361-8.
Hutchings A, Raine R, Sanderson C et al. (2006) A comparison of formal consensus methods used for developing clinical guidelines. J Health Serv Res Policy, 11(4): 218-24.
Institute of Medicine (2001) Crossing the quality chasm: A new health system for the 21st century, Washington, DC: National Academies Press.
Johnston R, Clark G (2005) Service operations management: improving service delivery. 2nd Edition, Pearson Education: Prentice Hall.
Jones J, Hunter D (1995) Consensus methods for medical and health services research. BMJ, 311(7001): 376-80.
Kaushal R, Shojania KG, Bates DW (2003) Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med, 163(12): 1409-16.
Kitzinger J (1995) Qualitative research. Introducing focus groups. BMJ, 311(7000): 299-302.
Lehnert BE, Bree RL (2010) Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: how critical is the need for improved decision support? J Am Coll Radiol, 7(3): 192-7.
MacKenzie R, Sims C, Owens R et al. (1995) Patients' perceptions of magnetic resonance imaging. Clin Radiol, 50(3): 137-43.
Nelson CW, Niederberger J (1989) Patient satisfaction surveys: an opportunity for total quality improvement. Hosp Health Serv Adm, 35(3): 409-27.
Ponsignon F, Smart P, Maull R (2011) Service delivery system design: characteristics and contingencies. International Journal of Operations & Production Management, 31(3): 324-49.
Porter ME, Teisberg EO (2004) Redefining competition in health care. Harv Bus Rev, 82(6): 64-76.
Rosenthal DI, Weilburg JB, Schultz T et al. (2006) Radiology order entry with decision support: initial clinical experience. J Am Coll Radiol, 3(10): 799-806.
Singh H, Arora HS, Vij MS et al. (2007) Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc, 14(4): 459-66.
Törnqvist E, Månsson Å, Larsson EM et al. (2006) It's like being in another world–patients’ lived experience of magnetic resonance imaging. J Clin Nurs, 15(8): 954-61.
Vaartio-Rajalin H, Leino-Kilpi H (2011) Nurses as patient advocates in oncology care: activities based on literature. Clin J Oncol Nurs, 15(5): 526-32.
Vanhaecht K, Panella M, van Zelm R et al. (2010) An overview on the history and concept of care pathways as complex interventions. International Journal of Care Pathways, 14(10): 117-23.
Vanhaecht K, De Witte KD, Depreitere R et al. (2006) Clinical pathway audit tools: a systematic review. J Nurs Manag, 14(7): 529-37.
Von Korff M, Goldberg D (2001) Improving outcomes in depression. BMJ, 323 (7319): 948-9.
Ware GW (2003) Patient satisfaction surveys. Optometry, 74(10): 671-4.
Yazdanparast A, Manuj I, Swartz SM (2010) Co-creating logistics value: a service-dominant logic perspective. International Journal of Logistics Management,21(3): 375-403.










