HealthManagement, Volume 2 - Issue 2, Winter 2008
Equitable access to healthcare forms one of the common objectives for EU Member States in the fight against social exclusion and poverty, yet barriers remain in the way of goals for optimum and homogenous access. For medical technologies, these barriers to access can be multi-factorial, yet broadly classified as stemming from the supply or demand side.
In
this article, within the focus of cardiovascular device implantation, we
examine trends in the disproportions of access to innovative technologies and
survey their possible influencing factors. Our objective
is to briefly recapitulate findings fromthe
literature on the prevalence of thisproblem
in Europe to feed into policydiscussions on
optimisation and homogeneityof device
implantation access.
Variability and Inequality Despite Guidelines
Variability in the access to cardiovascular technologies has been observed to occur at many levels in Western Europe, from international to local. For example, there is strong evidence indicating a high level of variability among Western European countries in the per-million utilisation of cardiovascular technologies despite commonly accepted management guidelines for their use. In contrast, disparities of access at local levels have also been measured within given regions.
Underutilisation forms another type of disparity when there are
gaps between the true or projected incidence of need and actual rates of
utilisation. When this occurs, the situation implies that not all patients
within a local population with need for the technology are guaranteed access to
it. Each of these situations in which unequal access occurs is surveyed in the
current article.
Eucomed Data on Implant Rates Shows Disparities
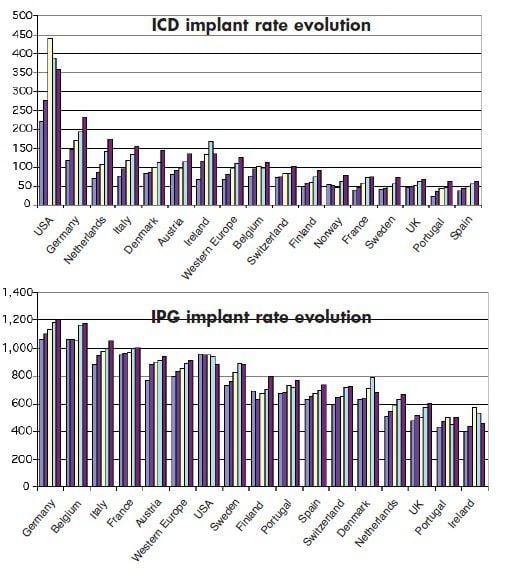
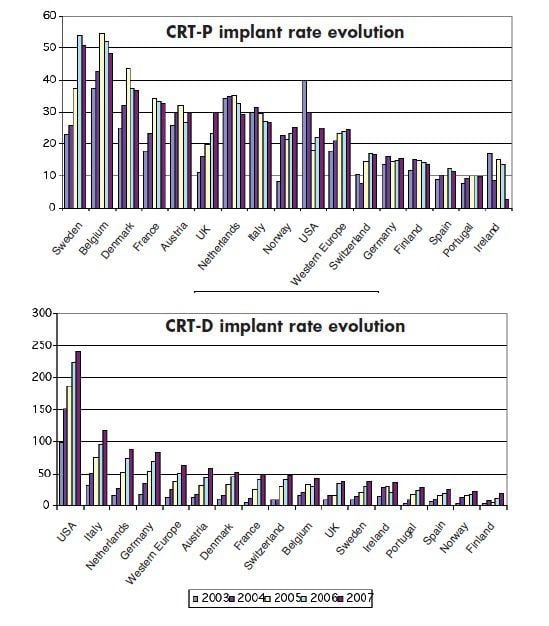
On an international level, key data on cardiovascular device implant rates and trend comparisons between European countries and the US have recently been published by EUCOMED illustrating large disproportions in access patterns. These trends can be observed in the figures illustrating implantation rate evolutions. While an overall growth trend has been observed for all types of implants including ICDs, CRTs and IPGs across countries, actual implant rates per million patients have been shown to vary extensively with the exception of IPGs, for which there is less variability.
In this regard it has been noted that internationally recognised guidelines for pacemaker implantation and the dissemination of evidence-based findings have led to reduced differences between European and North American practices in the treatment of brady cardias and specifically by pacemakers. The same researchers propose that this variability may be underpinned by differences in the proportion of GDP comprising healthcare expenditure, as well as discrepancies in the demographically- adjusted availability of practicing cardiologists and implant centres.
Access Rates Tied to WealthNot Disease Burden
Key studies in Europe on inter-region and inter-hospital variability have been led in Spain and the UK and confirm the existence of variability of access to cardiovascular technology for both diagnosis and treatment. Specifically in Spain, the use of coronary angiography is related to the wealth of the autonomous region, but not to the disease burden.
Other studies reveal disparities of cardiovascular device implant access and focus on numerous variables including supply, demand, regional wealth, and resources allocated to healthcare. Such work has shown that there is strong regional variability in the use of PCI, ICD and CRT, and that this variability is higher the more recently available the procedure.
For example, the ratio of variation between the maximum and
minimum number of procedures done, ranges between almost double (1.95) for PCI,
introduced in Spain in the 1980s, triple (3.04) for ICD, which became available
in the 1990s, and above 15 (15.7) for CRT devices available at the end of the 1990s. Implant rates were also strongly associated with
supply-driven variables including the number of centres that provided the
procedure and the number of qualified implant specialists.
UK Group Paints Alarming Picture for Cardiac Patients
In the UK, the Cardiac Network Device Survey Group has recently reported an alarming picture for cardiac patients in the NHS where it exposes major inequity of provision (“postcode prescribing”) between networks and primary care trusts for all classes of device and for pacemaker mode prescription. Furthermore, cardiac device implantation rates are amongst the lowest in Western Europe despite evidence refuting any difference in the prevalence of conditions for which implantation is indicated or the over-prescription of devices in other countries. The report also suggests some proposals to overcome these inequities:
- Investment in implanting and follow- up services, and in education of health professionals at all levels of the referral chain to ensure that the ability to recognise, refer and act upon an indication for device implantation is optimised; and
- The implementation of clinical pathways enabling the systematic identification and early assessment of potential candidates to improve the uptake of primary prevention device therapy.
Finally, under provision of cardiovascular device implantation services has been cited in a number of recent studies conducted across Europe. These under provisions, as based on the magnitude of gaps between incidence rates and actual implant rates, are normally estimated as a proportion of the actual number of procedures conducted compared to the number of indications in a population.
Under-Provision of ICD Therapy in the UK
One recently conducted UK single-centre study observed significant
under-provision of ICD therapy in the UK. This conclusion was based on an
estimation of a combined projected ICD indication incidence (approximately 105
- 115/million/ year) using published data for NICE secondary prevention
indications as a benchmark and compared with the latest published UK ICD
implantation rate data (of approximately 40/million/year). This significant
level of under-use is comparable with other cardiovascular services in the UK,
for which the consequences have included higher morbidity and mortality rates. Separate
studies in cardiovascular services in the UK have noted that constraints on
costs were less likely to influence the decision to perform the procedure in a national
health system as compared with a private healthcare market. Additional studies
have also found strong correlation between ethnicity and access rates (adjusted
for age, socio-economic status, and physician bias) with some ethnic groups less
likely to receive cardiac procedures. Women also have been affected by age differences
in cardiovascular management.
Conclusions
At all levels the potential costs to societies are high from disparities in access to cardiovascular technologies; these disparities either manifesting as variability among populations or inequity within a population. The problem is an especially significant cause for concern in the cardiovascular indication given the enormous epidemiological burden of cardiovascular disease, its deadly health consequences and its high attendant costs.
Furthermore, the importance of homogeneity in the access to cardiovascular device implants such as CRTs, IPGs and ICDs is underscored by the incidence of sudden cardiac death which is a major health concern in developed countries, claiming more lives each year than stroke, lung and breast cancer, and AIDS combined. Given the potential these devices have in increasing patients’ chances of survival, policy discourse on healthcare equity must question the current patterns of device implant access, as revealed in numerous studies in the literature, and consider reallocation of resources supporting these innovative technologies.
References:
References used in this article are available on request to the Editor at: [email protected]





