The 2024 ESC Guidelines for the management of atrial fibrillation (AF), developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS), introduce new approaches and treatment-specific recommendations to address the growing number of AF patients worldwide.
Atrial fibrillation is one of the most prevalent heart conditions, impacting healthcare services across all levels of care, from primary to tertiary. Due to an ageing population, an increasing burden of comorbidities, greater awareness, and advancements in detection technologies, the prevalence of AF is expected to double by 2050.
AF affects patients differently, but the associated morbidity remains a significant concern. Patients with AF often experience various symptoms and a reduced quality of life. While stroke and heart failure are well-recognised complications, AF is also linked to other thromboembolic outcomes, including subclinical cerebral damage (potentially leading to vascular dementia) and embolism to other organs, contributing to the increased mortality risk associated with AF.
The 2024 guidelines emphasise optimal care through the new AF-CARE pathway, designed to ensure that all AF patients benefit from recent scientific advancements: [C] Comorbidity and risk factor management; [A] Avoid stroke and thromboembolism; [R] Reduce symptoms through rate and rhythm control; and [E] Evaluation and dynamic reassessment.
The guidelines highlight the importance of shared decision-making involving both patients and a multidisciplinary team in treatment choices and care planning. Education of patients, their families, and healthcare professionals is prioritised to empower informed treatment decisions tailored to each patient. There is also a strong focus on equitable care, emphasising the need to avoid disparities based on gender, ethnicity, disability, or socioeconomic status.
The comorbidities section of the new guidelines underscores that AF should not be viewed in isolation. Comprehensive evaluation and management of comorbidities and risk factors are crucial in all aspects of AF care to prevent recurrence and progression, enhance treatment success, and reduce AF-related adverse outcomes. There needs to be a greater focus on conditions and lifestyle factors with emerging evidence of their impact on AF and patient care.
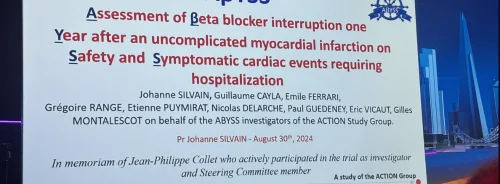
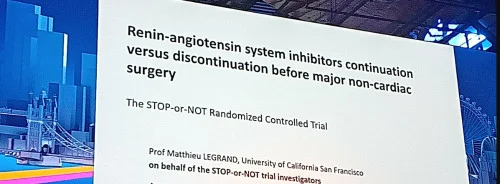
The guidelines also incorporate findings from recent clinical trials and studies that have the potential to improve routine management of AF patients. Key new features include:
- Broader use of appropriate anticoagulant therapy with the CHA2DS2-VA score (excluding gender) for decision-making.
- A 'safety-first' approach, such as delaying cardioversion if AF duration exceeds 24 hours and thoroughly evaluating potential side effects of antiarrhythmic drugs.
- Integrating rate and rhythm control with shared decision-making on referrals for catheter and surgical ablation.
The authors emphasise the need for ongoing evaluation and reassessment of patients with AF, stating: "Healthcare teams in primary and secondary care must periodically reassess therapies and focus on new modifiable risk factors that could slow or reverse AF progression, enhance quality of life, and prevent adverse outcomes."
Source & Image Credit: ESC Congress 2024