According to a recent survey by the Health and Social Care Information Centre, 43 percent of men and 50 percent of women in England are taking at least one prescription medicine, and 22 percent of men and 24 percent of women are taking at least three prescriptions. Nearly 2.7 million prescriptions are dispensed every day in England. This translates into an annual cost of £15 billion.
There is no doubt that the way doctors prescribe medicines has changed. There was a time when doctors prescribed statins to patients who had suffered a heart attack or stroke. The medication was part of secondary prevention, but statins are now used more liberally to prevent disease based on cholesterol levels and an evaluation of other risk factors such as blood pressure, body weight and ethnic origin.
Doctors now commonly use risk calculators such as Qintervention, which calculates an individual's risk of heart attack or stroke based on their cholesterol ratio, blood pressure and height-weight ratio. While some may perceive the risk of taking statins higher than their potential benefit, there are many who will take a chance on the statin's side effects in the hope that the medicine will reduce their risk of heart disease.
Secondary prevention has taken a back-seat and now it is all about preventing something that has not happened, turning healthy people into patients. While preventative measures such as vaccination, improved sanitation and food laws, and reducing smoking have helped improve the health of the population, preventative medication is sometimes misused. Everyone over the age of 40 is now being offered a five-year health check and about a half of screened people end up being prescribed a statin.
There is no concrete evidence that preventative medication as a health intervention actually works. A Cochrane review and another randomised trial in Denmark found no evidence of efficacy. Public Health England has also stated that it is being done “in the absence of direct randomised controlled trial evidence to guide it.”
This practice of over-prescribing and relying on pill-taking to improve the overall health of the population is a risky proposal. There is no guarantee that people will continue to take these long-term medications. In addition, research shows that people who take tablets most regularly live the longest, whether they are taking an active drug or a placebo. In other words, if millions are invested on statins, the benefits of the medicine will go to those who are already likely to live the longest. However, there is no logic in prescribing them with medications that could have negative side-effects.
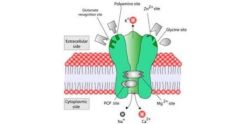
Another problem is that of "polypharmacy". Many people now take multiple medications that could react with one another. Approximately 6.5 percent of hospital admissions are due to the side-effects of medication. To make matters worse, a majority of people taking multiple medications are older and more frail.
Doctors are being judged on the volume of their prescribing. This should not be the case. The objective should be to provide quality care to patients and to make sure they make informed choices about medications. Overselling pharmaceuticals is not the goal of effective healthcare.
Source: Guardian
Image Credit: Wikimedia Commons